What is Osteoporosis?
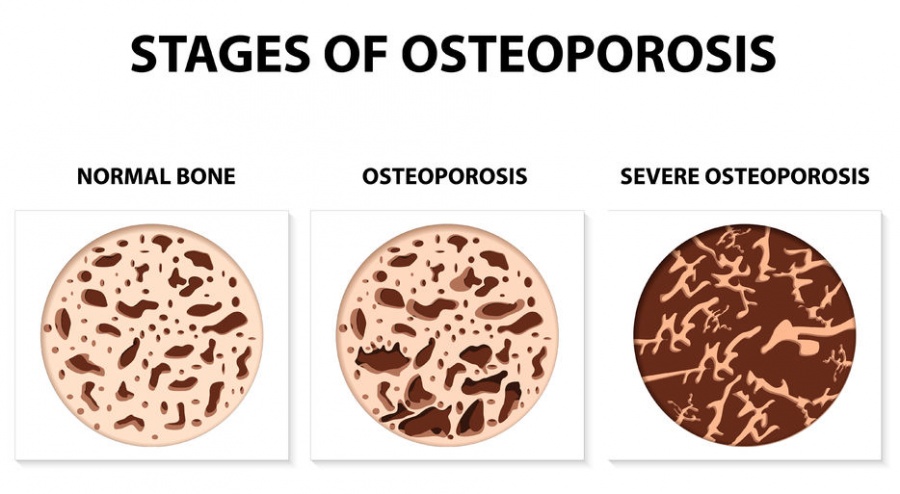
Osteoporosis is a disease of the bones. It occurs when the bones lose their normal density, become more porous, and become more fragile or brittle. This disease increases the chances of a broken bone, especially a break without significant trauma (ie. ground level fall).
What are the signs and symptoms of osteoporosis?
Osteoporosis does not have any specific signs or symptoms and is often considered a “silent disease.” Most people do not know they have osteoporosis until they break a bone. The most common types of fractures due to osteoporosis are vertebral fractures, hip fractures and wrist fractures.
How common is osteoporosis and who gets it?
Nearly 10 million Americans have osteoporosis and even more than that have osteopenia. Osteopenia is low bone density that does not severely weaken the bones like osteoporosis does, but it does place patients at an increased risk for developing osteoporosis. Although osteoporosis can arise at any age, it is more common in the elderly population. Many people think osteoporosis is a disease only women can get, but men can get osteoporosis too. About 50% of women and 25% of men over 50 years old will sustain an osteoporotic fracture in their lifetime.
What are the risk factors for osteoporosis?
There are multiple risk factors for osteoporosis. Postmenopausal women are at highest risk to develop osteoporosis. Estrogen levels decline after menopause and low estrogen levels leads to loss of bone mass. Some other major risk factors are increased age, sedentary lifestyle, genetic family history, smoking, drinking alcohol, long-term steroid use and a diet low in vitamin D and calcium. A lot of these risk factors are obviously not preventable, but there are things we can do to decrease the chances of osteoporosis. There are also many diseases and secondary causes of osteoporosis, such as kidney failure, anorexia/bulimia, rheumatoid arthritis, multiple sclerosis, Cushing’s disease, hyperthyroidism, hyperparathyroidism and diabetes. Treating these medical conditions is important to reverse or slow down the progression of osteoporosis.
What are the complications of osteoporosis?
The most devastating complication of osteoporosis is a bone fracture. Fractures can be extremely detrimental to one’s health. Fractures can mean a hospital stay, surgery and limited mobility. All of these things can increase the chances of other health issues like blood clots, pneumonia, etc., resulting in decreased quality of life. Another complication of osteoporosis is interference with orthopedic surgery. Many orthopedic surgeries require strong healthy bones to be successful including total joint procedures, fracture repairs and spinal fusions. Osteoporotic bone can increase the complexity of the surgery and failure rate of these procedures, thus putting the patient at higher risk for surgical failure and possibly more surgeries.
Fractures can mean a hospital stay, surgery and limited mobility. All of these things can increase the chances of other health issues like blood clots, pneumonia, etc., resulting in decreased quality of life. Another complication of osteoporosis is interference with orthopedic surgery. Many orthopedic surgeries require strong healthy bones to be successful including total joint procedures, fracture repairs and spinal fusions. Osteoporotic bone can increase the complexity of the surgery and failure rate of these procedures, thus putting the patient at higher risk for surgical failure and possibly more surgeries.
What can I do to prevent osteoporosis?
Osteoporosis can be avoided or delayed by maintaining a healthy exercise and diet regimen. This should be started at a young age and continued throughout your life. It is also very important to consume enough calcium and vitamin D. Calcium and Vitamin D can be consumed in pill/supplement form if you are not getting enough in your diet. Weight bearing exercises and resistance exercises, including walking and lifting weights, can help slow down the progression of and even prevent the onset of osteoporosis. Although it is important to start early in life and maintain a healthy lifestyle, it is never too late to work on preventing progression of osteoporosis. Other important things that you can do are quit smoking and limit caffeine intake. Hormone replacement therapy (HRT) after menopause can also help prevent osteoporosis due to the direct relationship between low estrogen and osteoporosis. All medications should be discussed with your team of physicians, as most come with other risks or side effects. It could also be important to discuss significant changes to your lifestyle or diet with your team of physicians to be sure your choices are safe for you.
How do I know if I have osteoporosis?
Early diagnosis of osteoporosis is very important because there are ways to help slow the disease’s progress or even reverse the disease. Your primary care physician or Rheumatologist will evaluate you with a physical exam, lab tests and also assess your risk factors for osteoporosis. It is also important for your health care provider to rule out any secondary causes of osteoporosis as detailed above. A diagnosis of osteoporosis is made with a Bone Mineral Density (BMD) test which evaluates your personal bone density.
How is it treated?
Although getting enough calcium and vitamin D can help prevent further bone loss, this usually not enough to treat the disease by itself. As stated above, lifestyle changes including proper diet and weight bearing exercises can help increase bone mass. As far  as clinical treatment for osteoporosis, Estrogen is an option for postmenopausal women to help slow bone loss and increase the body’s calcium stores. It is important to remember that this hormone does not come without possible side effects. There are many other different medications out there, the most common being Bisphosphonates. These drugs are capable of slowing bone loss, increasing density of bone and decreasing the changes of osteoporotic fractures. There are many other medications and you should discuss with your physician which one is right for you.
as clinical treatment for osteoporosis, Estrogen is an option for postmenopausal women to help slow bone loss and increase the body’s calcium stores. It is important to remember that this hormone does not come without possible side effects. There are many other different medications out there, the most common being Bisphosphonates. These drugs are capable of slowing bone loss, increasing density of bone and decreasing the changes of osteoporotic fractures. There are many other medications and you should discuss with your physician which one is right for you.
By Bethany Wink PA-C