What is a herniated disc?
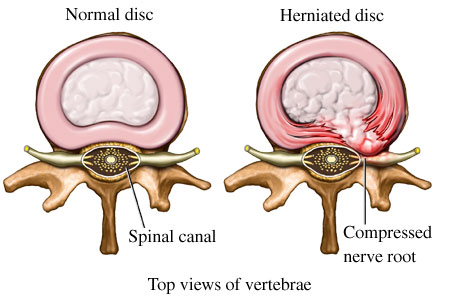
A herniated disc is when material from a vertebral disc ruptures into the spinal canal. Your spine is made of up a column of vertebrae separated by discs. Your nerves runs down behind the column of vertebral bodies and discs. You can think of the discs like a jelly donut. The outer shell (donut dough) can break open and let some of the jelly (inner disc material) stick out. The rupture of this jelly-like material into the canal can compress the nerves in the spine, causing significant leg pain, numbness, tingling and/or weakness. Herniated discs can occur anywhere along the spinal column. The most common location is in the lumbar (lower back) area, which is what the rest of this article will focus on.
What are the causes and risk factors of a herniated disc?
Herniated discs can be due to injury or due to the normal aging process of the spine. Different risk factors that increase your chance of having a herniated disc include male gender, genetic predisposition, obesity, repetitive heavy lifting, improper lifting mechanics, repetitive bending/twisting, prolonged/frequent driving, sedentary life and smoking. Although there are a few risk factors that cannot be avoided, like genetic predisposition, practicing a healthy lifestyle and proper lifting mechanics can decrease your chances of a herniated disc.
What are the symptoms of a herniated disc?
Symptoms of a herniated disc can vary and may be different, depending on where in the spine it occurs. Herniated discs can cause back pain, but they more commonly cause pain, numbness and/or tingling down one or both legs. This feeling is referred to as “sciatica” by many patients. The pain is usually described as a sharp, stabbing or burning pain. It is commonly made worse with sitting, coughing and/or sneezing. Weakness in a leg and/or foot is another common symptom of a herniated disc.
What should I do if I think I have a herniated disc?
If you have back and/or leg pain that persists, you should make an appointment with either your Primary Care Physician or a spine specialist. They will take your history and perform an exam on you to help determine the cause of the symptom(s). Figuring out the underlying cause is important, because the symptoms of a herniated disc can be similar to other issues that benefit from different treatment options. The exam will test the strength, reflexes and sensation in your legs. They may also ask you to walk to assess your gait. Based on your history and exam, the physician may offer you a treatment plan or send you for further testing.
What types of tests might my physician order?
The types of tests that are ordered and when they are ordered will vary, depending on your history and exam. At your first visit to a spine specialist, they will likely order x-rays for a baseline reading. The x-ray will likely show decreased disc height; however, this finding does not necessarily mean there is a disc herniation. The best test to confirm the diagnosis of a herniated disc is magnetic resonance imaging, or MRI. An MRI helps to figure out the extent of and exact location of the herniation. Knowing the exact location is important for targeting treatment. Some patients are unable to get an MRI due to different reasons (ex. pacemaker) in which case a CT myelogram would be ordered instead. A radiologist injects dye into the patient’s spinal canal and a CT scan is then performed. This test is a good alternative to an MRI to assess herniated discs.
What are the different treatments for a herniated disc?
Complete resolution of symptoms can be achieved with conservative management alone.
Different conservative treatments include: physical therapy, NSAIDS (ex. Ibuprofen, Naprosyn), short term steroid therapy and epidural steroid injections. Physical therapy concentrates on core strengthening to counter-balance the strain on the back in day-to-day activities. It also focuses on stretching, to improve range of motion and reduce stress on the low back. NSAIDS and oral steroids help decrease the inflammation within and around the nerve which can decrease the irritation and pain. Epidural steroid injections can significantly improve the patient’s symptoms by injecting steroids around the affected nerve using a needle and CT guidance. Although epidural steroid injections are invasive, they allow some patients to get significant relief while avoiding surgery. It is important to note that most herniated discs resolve without any permanent issues.
Conservative treatment can lead to symptom improvement within the first 6 weeks of a herniated disc. Patients can continue to improve for months with conservative treatment. Therefore, 6 weeks of conservative treatment is usually suggested prior to MRI or surgery for patients who do not have symptoms causing a neurologic deficit (i.e. weakness).
Surgical repair of a herniated disc may also be an option. Surgery can allow for quicker results and a faster recovery. But, it is important to understand that the same final recovery is likely achievable with conservative treatment options over a longer period.
Narcotics are typically not prescribed for herniated discs. If they are necessary, they should only be a short-term treatment.
When should I consider surgery?
Surgery should be considered when symptoms do not improve after 6 weeks of conservative treatment. If you are having persistent symptoms for longer than 6 weeks, surgery can provide more rapid relief to improve your quality of life.
Surgery should be considered emergently when there is neurologic deficit. Neurologic deficits include paralysis or progressive leg weakness, decreased or absent reflexes, numbness or tingling in the genital region, or bowel or bladder dysfunction (impotence or incontinence). Any of these symptoms or a combination of these symptoms is an emergency and requires immediate surgery to avoid 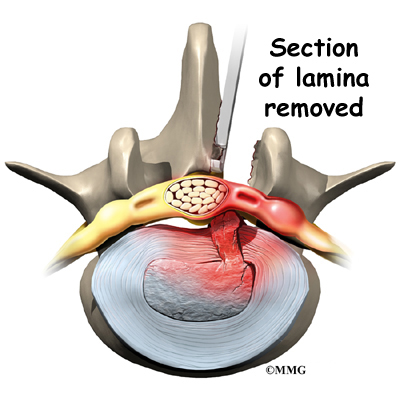 permanent issues.
permanent issues.
The most common procedure for a lumbar disc herniation is a microdiscecromy. A small incision is made in the lumbar spine. The muscle and tissues are dissected away. A small portion of the bone (lamina) is removed from the lumbar spine to get to the herniated disc. The ruptured piece of disc is carefully removed.
What is the recovery like after a microdiscectomy?
Patients usually notice a decrease in their leg pain after a microdiscectomy. Sensation and strength deficits may take a bit longer to return. If there is prolonged weakness prior to surgery, it may not fully resolve. Overall, patients can continue to feel better for months after surgery.
What are the risks of a microdiscectomy?
One of the more common risks after disc surgery is a re-herniation. This occurs about 5-10% of the time. Only the ruptured piece of the jelly-like disc is removed during surgery, so there is a chance another piece can rupture out of the same area. Other risks of surgery include infection, bleeding, spinal fluid leaks, and nerve damage, but these are rare. There is usually not enough bleeding during a microdiscectomy to cause severe issues or result in a blood transfusion. Nerve damage is very rare; careful technique is used to ensure that this does not occur. A spinal fluid leak is a tear in the outer covering of the nerves, which can usually be repaired during the original surgery. But, this may cause you to be placed on bed rest for a few days to help the leak to heal. Overall, the risks that go along with a microdiscectomy are rare.
The orthopedic spine specialists at Three Rivers Orthopedics are here to help you if you are having back pain or think you may have a herniated disc. Call 412-782-3990 to make an appointment today!
By Bethany Wink PA-C