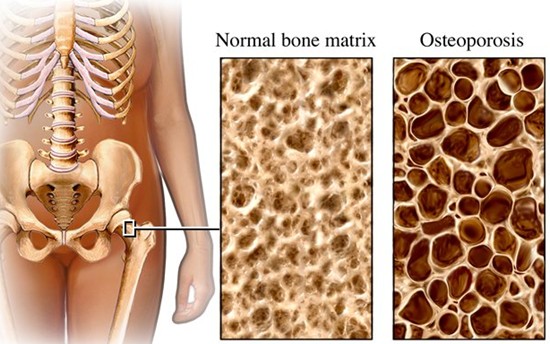
Osteoporosis
A major cause of disability in older adults is often due to fractures that limit mobility and interfere with activities of daily living. Fractures are common amongst elderly individuals for a multitude of reasons. One of the most common being osteoporosis. Osteoporosis is defined as a condition in which the body loses too much bone or makes too little bone, resulting in the bones becoming brittle and weak. The word osteoporosis literally means “porous bones.” You can find more information about osteoporosis by scrolling down in the “News and Events” section of the website where an article on this disorder was previously posted.
Risk Factors for Decreased Bone Density
As we age, our bone quality and bone mass decreases. Some non-modifiable risk factors that lead to a reduction in bone mass include: advanced age, female sex, family history of osteoporosis or hip fracture, certain metabolic disorders, and certain types of malignancies such as lymphoma or myeloma. Metabolic disorders that can lead to osteoporosis include hyperthyroidism, type 1 diabetes, vitamin D/calcium deficiency, or alcoholism to name a few. Some modifiable risk factors that lead to decreased bone mass include smoking, low calcium intake per diet, low vitamin D level from lack of sunlight, sedentary lifestyle, and steroid therapy.
Incidence of Osteoporosis
The prevalence of osteoporosis increases dramatically as age increases. According to the World Health Organization, 13-18% of women in the US older than 50 years have osteoporosis and 37-50% have osteopenia, which is defined as a reduction in bone mass to a lesser severity than osteoporosis. As for men, 3-6% have osteoporosis, while 28-47% are osteopenic. Osteoporosis is more common in women due to hormonal changes that occur secondary to menopause. Fracture risk can be reduced with early identification and treatment of osteopenia and osteoporosis. It is suggested that any patient with a low-trauma, or low-impact type of fracture should be worked up and have their bone density evaluated.
Risks and Complications Associated with Osteoporotic Fractures
Fractures that occur in the setting of osteoporosis include hip fractures most commonly, vertebral fractures in the back, and wrist fractures. The complications related to immobility caused by these fractures are of grave concern. The loss of functional activity and quality of life that results, mostly with hip and vertebral fractures increases the likelihood of illness and risk of death among affected patients. For example, according to the US surgeon general, the risk of death during the first 3 months after hip fracture is 3-4 times greater than patients who do not sustain hip fractures. It has been reported that 20 percent of patients will die within a year of the hip fracture due to complications from immobility and another 20 percent end up in a nursing home within that year.
Why Fractures Occur in the Setting of Normal Aging and Osteoporosis
Our bodies have a normal balance of bone turnover, repair, and replacement that occurs normally every day. In the setting of menopause due to hormonal changes, this normal balance is disturbed. The balance of bone turnover is also disturbed during the normal aging process, as well as in other disorders as mentioned above. The cells involved in this process are called osteoblasts and osteoclasts. Osteoclasts break down old bone tissue whereas osteoblasts replace it with new bone. Together, these cells facilitate bone healing and bone growth. In the above mentioned circumstances, osteoclasts cause more bone to be lost than osteoblasts are able to restore, resulting in weakened bones and increased risk for fractures.
Preventing Fractures
In this segment, the focus will be more about preventing fractures before a diagnosis of osteoporosis has been made. There are a number of pharmacological treatment options out there for osteoporosis that would be managed by a primary care physician or rheumatologist for the management of this disease. Here, the focus is more about education on the non-pharmacologic strategies to increase bone health, prevent fractures, and recognize risk factors for the development of osteopenia or osteoporosis. Listed below are some strategies to improve bone health and reduce the risk of fractures.
–Combined calcium and vitamin D intake – calcium alone has not been shown to reduce fractures: The recommended dosage is 1,200mg per day of calcium (either from diet or supplementation) and 800-1,200IU per day of vitamin D. Foods that are good sources of calcium include: yogurt, milk, cheese, spinach, and collard greens.
-Weight-bearing exercise – examples include: running, walking, jumping rope, stair climbing, and progressive resistive exercises such as lifting weights. These types of exercises are important because they improve strength, balance and coordination and help reduce the risk of falls, which often result in fractures in the elderly population.
-Consume less caffeine – too much caffeine can interfere with the body’s ability to absorb calcium.
-Quit smoking – besides all of the well-known detriments to health that smoking causes, it also has a negative impact on bone health and bone quality, by preventing the body from adequately absorbing calcium
-Limit alcohol intake – studies have shown that excessive alcohol intake can cause bone loss as it interferes with vitamin D doing its job in the body. Although, recent studies show that light alcohol consumption (1 drink per day for women and 2 drinks per day for men) may actually slow bone loss.
-Medication review – some medications or a combination of different medications may cause drowsiness, or light-headedness which may lead to falls. It is important to have your primary care doctor review your medications.
-Vision screens – yearly visual checks are important to make sure your prescription is accurate. It is also important to rule out age related conditions such as glaucoma or macular degeneration that may impede vision.
-Make sure your home is safe – Remove all small area rugs or other items on the ground that you can trip on. Avoid using step stools. Install non-slip mats in the bathtub or shower. Add handrails on all staircases. Assure good lighting in all rooms. Lastly, wear supportive shoes with non-slip soles over slippers in the home.
For more information about fall prevention and programs for the elderly, visit your local YMCA or gym or talk with your physical therapist in regards to a balance and strengthening program.